Abstract
Abstract
Purpose: To evaluate the value of single nucleotide polymorphism array (SNP-A) analysis on the diagnosis and prognosis of Chinese patients with myelodysplastic syndromes (MDS).
Methods: 416 cases were recruited from two medical centers in China; of which 200 cases were diagnosed with MDS, 25 with myeloproliferative neoplasm (MPN), 63 with primary acute myeloid leukemia(AML), 40 with aplastic anemia (AA), 62 with idiopathic cytopenia of undetermined significance (ICUS), and 26 were healthy individuals. We analyzed chromosome abnormalities in all the cases with both SNP-A and metaphase cytogenetics (MC) methods, and evaluated their clinical significance as well. Clinical data analyzed included age, sex, blood counts, marrow morphology, blast counts, progression free survival (PFS) and overall survival(OS).
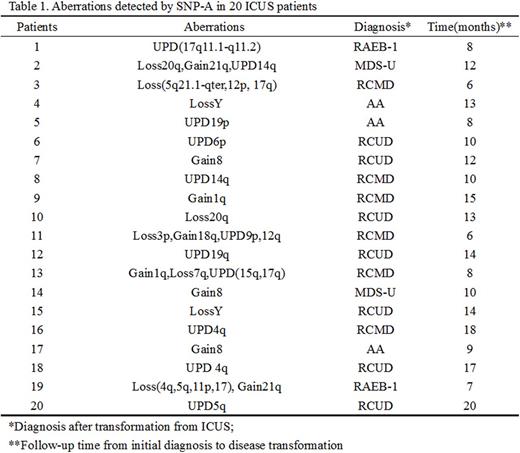
Results: 1. SNP-Aanalysis leaded to a significantly higher detection yield of chromosome abnormalities than MC examination. The abnormal detection rate for MDS, MPN and AML by MC was 42%, 48% and 36.5%, but by SNP-A significantly increased to 73.5%,72% and 69.8%, respectively. Moreover, SNP-A analysis revealed complex types and genomic distribution patterns of chromosome aberrations. 2. Notably, 20 of the 62 ICUS patients had abnormal detections by SNP-A, and interestingly 17 of these 20 ICUS patients with abnormal SNP-A detections transformed to typical MDS with a median follow-up time at 11months(Table 1). 3. Prognosis of the MDS patients with abnormal SNP-A detections was significantly worse than that of those patients without abnormal SNP-A observations in OS (24 months vs not reached (NR); P=0.004) and PFS (15 vs 40 months; P=0.002). Prognosis of the patients identified with abnormal SNP-A detections in addition to a normal or a good IPSS-R prognostic MC finding in a patient was significantly inferior than that of those patients with no such additional SNP-A aberrations in OS (25 months vs NR; P=0.004) and PFS (17 months vs NR; P=0.002). For the patients stratified as high-risk and very-high-risk MDS by the revised International Prognostic Scoring System(IPSS-R), there were no differences between the patients with and without SNP-A abnormalities in OS (13 vs 12 months; P =0.537) and PFS (14 vs 10 months; P =0.368); However, in the group of patients with very-low-risk, low-risk, and intermediate-risk MDS, the patients with SNP-A abnormalities showed significantly inferior survival than those without abnormal SNP-A detections in OS (NR vs NR; P=0.001) and PFS (25 months vs NR; P=0.008). 4. By multivariable analysis the presence of SNP-A aberrations additional to MC analyses in a patient and a higher number of SNP-A abnormalities (≥3 per patient) were independent predictors of poor prognosis for patients with MDS (HR=2.33, P=0.003; HR=2.40, P=0.002).
Conclusion:SNP-A analysis can help significantly improve the diagnosis and better evaluate the prognosis of patients with MDS, and help better assess the risk of MDS transformation in patients with ICUS. SNP-A analysis is of great practical value in clinical management.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.